Dental Emergencies
Dental Emergencies Contacts
William D. Titus, DMD, monitors an emergency cell phone after hours in case a patient of record requires emergency dental assistance.
This service if ONLY FOR PATIENTS OF RECORD*.
*A patient of record is one that has filled out our health questionaire and has been seen by Dr. Titus in the office at least once. Patients assigned to our office by certain dental plans are NOT patients of record unless they have been seen at least once and have a health questionnaire completed and signed.
*A patient of record is one that has filled out our health questionaire and has been seen by Dr. Titus in the office at least once. Patients assigned to our office by certain dental plans are NOT patients of record unless they have been seen at least once and have a health questionnaire completed and signed.
Restrictions on prescribing medications for individuals who are not patients of record and who have not been examined, require us to offer this service only to those who are established patients.
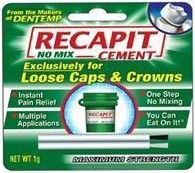
A dental emergency is considered: SEVERE IRRETRACTIBLE PAIN, SIGNIFICANT SWELLING, AIRWAY COMPROMISE, UNCONTROLLABLE BLEEDING, DENTAL TRAUMA, TOOTH AVULSION AND ALLERGIC REACTIONS. Lost crowns, either permanent or temporary, are not emergency situations. Commercially available temporary cements to reattach a crown are available at fine drugstores. Allowing a crown off over a weekend will not cause any problems.
IF YOU HAVE ANY DIFFICULTY IN BREATHING DUE TO SWELLING CAUSED BY A DENTAL INFECTION, PROCEED IMMEDIATELY TO THE NEAREST HOSPITAL EMERGENCY ROOM. IMMEDIATE MEASURES MUST BE TAKEN TO PREVENT AIRWAY OBSTRUCTION AND TO TREAT THE INFECTION. THIS SHOULD NOT AND WILL NOT BE HANDLED IN AN AMBULATORY SETTING.
IF YOU HAVE ANY DIFFICULTY IN BREATHING DUE TO SWELLING CAUSED BY A DENTAL INFECTION, PROCEED IMMEDIATELY TO THE NEAREST HOSPITAL EMERGENCY ROOM. IMMEDIATE MEASURES MUST BE TAKEN TO PREVENT AIRWAY OBSTRUCTION AND TO TREAT THE INFECTION. THIS SHOULD NOT AND WILL NOT BE HANDLED IN AN AMBULATORY SETTING.
Patients should be aware that dental visits which are outside of our normal business hours may result in an "after-hour" charge which can--under certain insurance plans--be as much as $150.00. This fee is in addtion to fees for procedures completed. Most insurance plans do not cover this fee and it is considered the patient's responsibility. This fee is in addition to other charges incurred at the time of the after hours emergency visit, such as x-rays, procedures and examinations, which may be a covered insurance benefit.
What to do When You Knock Out a Tooth
In the event you or a loved one knocks out a tooth because of some type of trauma, there are some things you should do right away. If the tooth has been avulsed completely and the root is not fractured, keep it moist. The cells on the root of the tooth should not be allowed to dry out or they will die. Dead cells on the surface of a tooth preclude it from being re-implanted into the socket.
It was once common to suggest placing the tooth in milk until a dentist could be consulted, and doing so is far preferable to allowing the tooth to dry out. However, milk is not readily available all the time and using such introduces foreign proteins, fats, milk sugars and the like onto the root surface. Commercially prepared kits to preserve knocked out teeth are available and any good sports medicine first aid kit should contain such. If, however, nothing is available, place the tooth into the cheek so saliva can continue to moisten and bathe the tooth. Better yet, if the root is not visibly dirty, try returning the tooth to the socket itself, that is if the socket is not distorted or crushed and it is not too painful.
You should contact your dentist for a tooth avulsion immediately so that the tooth may be returned to the socket and stabilized in some manner. Often, such teeth will reattached into the socket and continue to serve the patient. Avulsed teeth, however, have had their blood supply to the inner pulp broken, and as such, the inner soft pulp of the tooth will die. An avulsed tooth that is re-implanted into the jaw must have root canal therapy completed on it. Typically this will be done once the tooth is stabilized for a time and the attachment reforms. Some dentists will perform endodontic therapy on a tooth while outside of the mouth--keeping it moist all the while--and then return the tooth to the mouth.
It is important that when a tooth is re-implanted, that the tooth itself is stabilized in such a fashion that it has just a slight amount of movement to it or the tooth is more likely to ankylose--or become one with the bone. Often this means some wiring of the arch or even some orthodontic brackets.
Timely and proper treatment for a tooth avulsion is important to long-term success in retaining the tooth. While there is no guarantee than a tooth can be saved, once its knocked out, good success with re-implantation of teeth is common if the knocked out tooth is treated correctly and prompt re-implantation and stabilization is done.
It was once common to suggest placing the tooth in milk until a dentist could be consulted, and doing so is far preferable to allowing the tooth to dry out. However, milk is not readily available all the time and using such introduces foreign proteins, fats, milk sugars and the like onto the root surface. Commercially prepared kits to preserve knocked out teeth are available and any good sports medicine first aid kit should contain such. If, however, nothing is available, place the tooth into the cheek so saliva can continue to moisten and bathe the tooth. Better yet, if the root is not visibly dirty, try returning the tooth to the socket itself, that is if the socket is not distorted or crushed and it is not too painful.
You should contact your dentist for a tooth avulsion immediately so that the tooth may be returned to the socket and stabilized in some manner. Often, such teeth will reattached into the socket and continue to serve the patient. Avulsed teeth, however, have had their blood supply to the inner pulp broken, and as such, the inner soft pulp of the tooth will die. An avulsed tooth that is re-implanted into the jaw must have root canal therapy completed on it. Typically this will be done once the tooth is stabilized for a time and the attachment reforms. Some dentists will perform endodontic therapy on a tooth while outside of the mouth--keeping it moist all the while--and then return the tooth to the mouth.
It is important that when a tooth is re-implanted, that the tooth itself is stabilized in such a fashion that it has just a slight amount of movement to it or the tooth is more likely to ankylose--or become one with the bone. Often this means some wiring of the arch or even some orthodontic brackets.
Timely and proper treatment for a tooth avulsion is important to long-term success in retaining the tooth. While there is no guarantee than a tooth can be saved, once its knocked out, good success with re-implantation of teeth is common if the knocked out tooth is treated correctly and prompt re-implantation and stabilization is done.
Lost Temporary Crowns
Temporary crowns are made of plastic and as such, they flex when they are put under force while chewing. This is not a good situation, as the temporary cement that holds them on to the tooth can fracture and the crown can then come off the tooth. This is especially true for teeth that are short or when teeth hit hard--such as when individuals have no back teeth and they hit the front teeth hard. As such, it is not uncommon for temporary crowns to be lost before the permanent crown returns from the laboratory and can be permanently cemented.
Should your crown come off, call our office and we will do our best to re-cement it for you in a timely fashion. However, should this happen outside of office hours, we do not consider a lost temporary to be a dental emergency. While some sensitivity to hot and cold can be experienced when a temporary crown is lost, few if any lasting consequences arise if a tooth is left without a crown for a few days. While we do not like to leave the prepared tooth exposed for weeks--mainly because we fear tooth movement--allowing a temporary crown off a few days will rarely pose a problem.
Often, however, a lost temporary crown can pose a "cosmetic emergency". This is especially true when the tooth in question is a front tooth. Should your temporary crown still be in tact, you can easily re-cement it back on the tooth yourself. Several over-the-counter temporary crown cements are available for home use. Some of the brands are shown to the right.
To re-cement a temporary crown, clean the tooth itself of any remaining temporary cement and then the inside of the crown as well with a toothpick. Using cotton, rolled paper towels or gauze, dry the tooth while having someone mix the cement (if required by the type you get). Place the cement into the crown so that all inner walls of the crown are coated and about 1/2 the crown is filled with the material. Place it back onto the dried tooth and keep pressure on it for at least five minutes. You may then use a tooth pick and floss to remove the excess cement. Be sure when you floss, not to pull the floss back out through the contact, but release one end of the string and pull it out to the side.
We can then re-cement the crown for you during normal office hours should you not feel confident you obtained a good re-cementation. We regret that we cannot see patients for lost temporary crowns after hours, but doing so would be impractical, and after hour emergency appointments are prohibitively expensive. Lost temporary crowns are a headache for every dentist and many patients. Plastics used for temporary restorations just cannot endure some of the forces patients generate when chewing or clenching. Until better temporary materials are developed, they will continue to be problematic. Your patience in dealing with this temporary condition while your crown is being made, is appreciated.
Your permanent crown, being non-flexible and strong--along with the stronger permanent cement used under it--provides a much stronger type of cementation. Most permanent crowns, combined with permanent cement, cannot be removed and must be cut off should they ever needs to be removed. The experience with your temporary crown should not give rise to fear that the permanent crown may continue to fall out once its cemented permanently. Rarely is there such a problem.
In certain situations, we may even provide you with individually portioned temporary cement packets you can mix and use at home.
Should your crown come off, call our office and we will do our best to re-cement it for you in a timely fashion. However, should this happen outside of office hours, we do not consider a lost temporary to be a dental emergency. While some sensitivity to hot and cold can be experienced when a temporary crown is lost, few if any lasting consequences arise if a tooth is left without a crown for a few days. While we do not like to leave the prepared tooth exposed for weeks--mainly because we fear tooth movement--allowing a temporary crown off a few days will rarely pose a problem.
Often, however, a lost temporary crown can pose a "cosmetic emergency". This is especially true when the tooth in question is a front tooth. Should your temporary crown still be in tact, you can easily re-cement it back on the tooth yourself. Several over-the-counter temporary crown cements are available for home use. Some of the brands are shown to the right.
To re-cement a temporary crown, clean the tooth itself of any remaining temporary cement and then the inside of the crown as well with a toothpick. Using cotton, rolled paper towels or gauze, dry the tooth while having someone mix the cement (if required by the type you get). Place the cement into the crown so that all inner walls of the crown are coated and about 1/2 the crown is filled with the material. Place it back onto the dried tooth and keep pressure on it for at least five minutes. You may then use a tooth pick and floss to remove the excess cement. Be sure when you floss, not to pull the floss back out through the contact, but release one end of the string and pull it out to the side.
We can then re-cement the crown for you during normal office hours should you not feel confident you obtained a good re-cementation. We regret that we cannot see patients for lost temporary crowns after hours, but doing so would be impractical, and after hour emergency appointments are prohibitively expensive. Lost temporary crowns are a headache for every dentist and many patients. Plastics used for temporary restorations just cannot endure some of the forces patients generate when chewing or clenching. Until better temporary materials are developed, they will continue to be problematic. Your patience in dealing with this temporary condition while your crown is being made, is appreciated.
Your permanent crown, being non-flexible and strong--along with the stronger permanent cement used under it--provides a much stronger type of cementation. Most permanent crowns, combined with permanent cement, cannot be removed and must be cut off should they ever needs to be removed. The experience with your temporary crown should not give rise to fear that the permanent crown may continue to fall out once its cemented permanently. Rarely is there such a problem.
In certain situations, we may even provide you with individually portioned temporary cement packets you can mix and use at home.

Dental Infections
Swelling of the soft tissues of the face is often associated with an infected tooth. Once decay has entered into the soft center of the tooth, known as the pulp, bacteria can make their way into the bone. This can be a painful experience as pressure within the bone exerts pressure on the nerves which surround the teeth. Left untreated, the infection can "eat" its way out of the bone and begin to swell soft tissues.
Dental infections come in two varieties, a localized abscess that forms a pus epulis or a cellulitis, which is a more diffuse type of swelling. Epulis formation often produces swelling that is soft, warm, red and localized to a smaller area. In such cases, the pus from the infection can be drained and the patient is placed on antibiotics until the offending tooth is either extracted or treated with root canal therapy. In cases of cellulitis, where the infection is much more firm, diffuse and no focal point for pus formation is noted, the swelling cannot be drained. This type of infection--typically more severe--must be treated aggressively with antibiotic and a rapid treatment of the infection source. Patient that do not begin to see noticable improvement in 2 to 3 days after being placed on antibiotics must let their dentist know their antibiotic is not working. Some bacteria associated with tooth infection do not respond to first-line antibiotics and stronger antibiotics may need to be considered.
Swelling in certain areas is more dangerous than others. Swelling in the area of the upper eye teeth--called a canine space infection--can travel up about the nose. Concerns about cranial, secondary infections are warranted with this location, and prompt care is even more of a concern. Swelling with infected wisdom teeth can sometimes cause impairment of the airway because of swelling of the tongue or pharynx. This type of swelling can be life threatening and must be treated aggressively and promptly as well.
When you are first seen by a dentist, they may or may not recommend that the infection be drained. Drainage can be accomplished by opening the tooth and allowing exudate to flow out the root canal, or it may be achieved by incision for the swollen tissue. The treatment choice of either extracting the tooth or attempting to save it with root canal therapy is often the deciding factor. If the tooth can be removed at that first visit, drainage may not be necessary in all cases.
Any patient presenting with a dental infection will be placed on antibiotics and often pain medication as well. It is imperative that the patient be compliant in taking all of the antibiotic and to take it as prescribed. Even if the tooth is extracted or a root canal is completed, the antibiotic prescription should be finished. In recent years, the advent of antibiotic resistant bacteria has made the importance of doing complete rounds of antibiotic therapy all the more important. If you stop your antibiotic after only a couple of days of therapy, the strong bacteria may still be alive and viable. Such bacteria can reproduce and cause another infection that is more resistant to antibiotic than the first one.
If you are on antibiotic therapy for several days and see the infection worsening, you must contact the doctor who prescribed your antibiotic. Some bacteria are resistant to certain types of antibiotics and not changing the antibiotic in a timely fashion can lead to significant problems. As a rule of thumb, if after 48 hours of dosing on a particular antibiotic, the swelling does not begin to get better, you need to seek further help. In addition, patients can develop drug allergies to certain types of antibiotics that they have had on multiple occasions before. If severe itching, sudden reddening of the skin--with or without hives development--, difficulty breathing because of chest constriction, or a flushed feeling occurs soon after taking a dose of antibiotics occurs, you could be suffering from a severe allergic reaction. Go immediately to the hospital emergecy room with the aid of a family member or call 911. Slight itching, stomach upset or mild hives can indicate an early allergic reaction and the antibiotic should not be continued. You should contact your dentist for further instructions and a different antibiotic.
While saving an infected tooth is usually the best course of action, heavily damaged teeth that are not restorable or financial constraints often dictate a tooth must be extracted. Should the tooth appear to be a surgical extraction, you will most likely be referred to an oral surgeon. Infected teeth can be difficult to anesthetize and significant bone removal can make the procedure difficult. An oral surgeon who can do general anesthesia, concious sedation and who has many specialized instruments can make a difficult extraction much more pleasant for the patient. Whatever course of action you chose--to either remove a tooth or to save it with root canal therapy, it is important that the treatment be done promptly. Leaving infected teeth in the mouth will result in subsequent infections which can grow more severe with each onset. Repeatedly "hitting" an infection with antibiotics is not a good practice and is the primary cause for drug resistance in bacteria. As such, our office will only provide two rounds of antibiotics for any given dental problem. It is imperative that the patient work quickly to have the treatment planned procedure completed.
Dental infections come in two varieties, a localized abscess that forms a pus epulis or a cellulitis, which is a more diffuse type of swelling. Epulis formation often produces swelling that is soft, warm, red and localized to a smaller area. In such cases, the pus from the infection can be drained and the patient is placed on antibiotics until the offending tooth is either extracted or treated with root canal therapy. In cases of cellulitis, where the infection is much more firm, diffuse and no focal point for pus formation is noted, the swelling cannot be drained. This type of infection--typically more severe--must be treated aggressively with antibiotic and a rapid treatment of the infection source. Patient that do not begin to see noticable improvement in 2 to 3 days after being placed on antibiotics must let their dentist know their antibiotic is not working. Some bacteria associated with tooth infection do not respond to first-line antibiotics and stronger antibiotics may need to be considered.
Swelling in certain areas is more dangerous than others. Swelling in the area of the upper eye teeth--called a canine space infection--can travel up about the nose. Concerns about cranial, secondary infections are warranted with this location, and prompt care is even more of a concern. Swelling with infected wisdom teeth can sometimes cause impairment of the airway because of swelling of the tongue or pharynx. This type of swelling can be life threatening and must be treated aggressively and promptly as well.
When you are first seen by a dentist, they may or may not recommend that the infection be drained. Drainage can be accomplished by opening the tooth and allowing exudate to flow out the root canal, or it may be achieved by incision for the swollen tissue. The treatment choice of either extracting the tooth or attempting to save it with root canal therapy is often the deciding factor. If the tooth can be removed at that first visit, drainage may not be necessary in all cases.
Any patient presenting with a dental infection will be placed on antibiotics and often pain medication as well. It is imperative that the patient be compliant in taking all of the antibiotic and to take it as prescribed. Even if the tooth is extracted or a root canal is completed, the antibiotic prescription should be finished. In recent years, the advent of antibiotic resistant bacteria has made the importance of doing complete rounds of antibiotic therapy all the more important. If you stop your antibiotic after only a couple of days of therapy, the strong bacteria may still be alive and viable. Such bacteria can reproduce and cause another infection that is more resistant to antibiotic than the first one.
If you are on antibiotic therapy for several days and see the infection worsening, you must contact the doctor who prescribed your antibiotic. Some bacteria are resistant to certain types of antibiotics and not changing the antibiotic in a timely fashion can lead to significant problems. As a rule of thumb, if after 48 hours of dosing on a particular antibiotic, the swelling does not begin to get better, you need to seek further help. In addition, patients can develop drug allergies to certain types of antibiotics that they have had on multiple occasions before. If severe itching, sudden reddening of the skin--with or without hives development--, difficulty breathing because of chest constriction, or a flushed feeling occurs soon after taking a dose of antibiotics occurs, you could be suffering from a severe allergic reaction. Go immediately to the hospital emergecy room with the aid of a family member or call 911. Slight itching, stomach upset or mild hives can indicate an early allergic reaction and the antibiotic should not be continued. You should contact your dentist for further instructions and a different antibiotic.
While saving an infected tooth is usually the best course of action, heavily damaged teeth that are not restorable or financial constraints often dictate a tooth must be extracted. Should the tooth appear to be a surgical extraction, you will most likely be referred to an oral surgeon. Infected teeth can be difficult to anesthetize and significant bone removal can make the procedure difficult. An oral surgeon who can do general anesthesia, concious sedation and who has many specialized instruments can make a difficult extraction much more pleasant for the patient. Whatever course of action you chose--to either remove a tooth or to save it with root canal therapy, it is important that the treatment be done promptly. Leaving infected teeth in the mouth will result in subsequent infections which can grow more severe with each onset. Repeatedly "hitting" an infection with antibiotics is not a good practice and is the primary cause for drug resistance in bacteria. As such, our office will only provide two rounds of antibiotics for any given dental problem. It is imperative that the patient work quickly to have the treatment planned procedure completed.
DO NOT DO THE FOLLOWING IF YOU HAVE AN INFECTION CAUSED BY A TOOTH:
-
Do not put a heating pad on the swollen area because it eases the pain. Such can draw the infection to the heat source and a fistula can develop on the outside of the cheek, causing scaring.
-
Do not put aspirin on the swollen gum tissue and hold it there. This will cause an acid burn on the tissue, creating even more pain because of the traumatic ulcer.
-
Do not push on the swelling to get it to drain. This can spread the infection.
-
Do not take another person's antibiotics or just a few left over from before. The antibiotic may not be appropriate for a dental infection or you may contribute to a drug resistance in the bacteria. In addition, it is a felony and a federal offense to take a prescription not prescribed to you.
-
Do not hesitate in seeking prompt medical attention. Infections can destroy bone, cause nerve damage, create distant abscesses in the body, cause bacteremias (blood infections) and weaken the immune systems. Bacteria invasion of the body is a serious issue and while our immune system is actively fighting these invaders, there is a point where our body cannot keep up to the challenge. Any infection is a serious matter and it must be treated promptly.